We continue to add books to this section. If there is a particular book you would like to see included, let us know at info@mycarematters.org.
Reducing the Symptoms of Alzheimer’s Disease and other Dementias
A Guide to Personal Cognitive Rehabilitation Techniques (JKP Press 2019)
By Jackie Pool
The culmination of a life’s work, this book is full of advice to help you or your loved ones manage the wide-ranging symptoms of dementia, with practical information, clear explanations and innovative solutions to a huge variety of dementia-related issues. Jackie Pool has almost forty years’ experience in this field and was keen to share her knowledge and research with anyone facing a diagnosis, offering support and guidance and dispelling the many myths that surround the condition.
This book appealed to me not only because I know and admire Jackie Pool, but because she has clearly put so much of herself into its pages. It is far more than just a self-help reference book, at times it’s a deeply personal and autobiographical account of her own experiences in dementia care. Jackie skilfully guides us through the minefields of psychological theory and scientific research to ensure we are empowered in our understanding of the disease and therefore able to approach the symptoms with greater creativity, hope and positivity.
If we understand the changes happening in our brains, or those of our loved ones, then we are far less likely to feel anxious and vulnerable, knowledge is power. Jackie draws on many personal examples to shine a light on a huge number of topics from maximising sleep quality, to improving communication, understanding the role of prescription drugs, maintaining personal care, and exploring the different types of memory.
Using the latest cognitive rehabilitation techniques Jackie explains how our brains have the capacity to ‘re-learn’ old skills and master new ones, ‘bypassing’ the damage using a process called ‘Rementia’, a term originally coined by the late, great, Tom Kitwood. It is fascinating to read about Jackie’s eight-year dialogue with Professor Kitwood via a series of letters she initiated due to her concern that the more holistic ‘social’ approach mustn’t be at the expense of maintaining and enhancing cognitive function.
As a skilled occupational therapist, Jackie has always understood that the key to living well with dementia is to be given the tools necessary to keep active, engaged and as independent as possible rather than become prematurely de-skilled or ‘dis-abled’ by relinquishing too much and having everything done for you. The writer, Wendy Mitchell, has often said that if she lived with a partner, she would have struggled to have maintained the independent skills she still enjoys. We are all guilty of ‘doing’ too much for someone we care for simply because we feel we ought to, its quicker or feels safer to do so, when actually giving someone the tools to, for example, make their own cup of tea or dress themselves, is of far greater benefit both physically and emotionally.
Jackie is not afraid to broach some complex topics in this book including neuroplasticity, delirium, cognition and the science of nutrition, but in all these areas we are invited to simply take as much information as we need to further our own understanding with plenty of pointers to extend our reading and helpful infographics to make the content even more accessible. The latter part of the book provides some useful templates for making daily plans and aspirational targets including examples from Jackie’s own PAL (Pool Activity Level) instrument.
Throughout this book, Jackie never loses her conversational style, it succeeds in being an informative companion guide and one I would hugely recommend for anyone living with dementia or supporting others to live as well as they can with the condition.
By Anna C. Park
.
Dementia, Sex and Wellbeing
by Danuta Lipinska
Danuta has over 30 years experience supporting families, teaching, counselling and consulting on adult sexuality and dementia care. In this guide she brings her wealth of knowledge and insight to the fore, helping us to understand the cognitive impact of a dementia diagnosis on intimacy and relationships, and reminding us that our sexual identities and needs remain an integral part of who we are.

Her friendly conversational style makes this an incredibly enjoyable read as she expertly draws on her life’s work to aid our understanding of sexual behaviours as simply responses to a need for sensuality and intimacy rather than a ‘problem’ to be managed. The key message that our body and brain are one and ‘we separate them at our peril’ is central to this understanding. All our experiences, feelings, intimate moments and dreams are remembered by our bodies as much as our brains – therefore a dementia diagnosis does not mean a loss of physical knowledge and memory. A person can still consent to sexual intimacy without needing to know what day of the week it is because they still ‘know’ their husband and remember how it feels to be with them.
This is an illuminating read which embraces science, philosophy, psychotherapy and spirituality to help us to be more inclusive and self-aware in our conversations around sex and intimacy. After each chapter there are ‘Points for Reflection’ to guide discussions and chart shifts in our own understanding and responses. It highlights a real need for openness around sexuality and identity, someone may well reveal their true sexual self, following a move into care, after years of enforced repression. As Sally Knocker says in her Afterword: ‘It is rare to read a book where you feel that you have been in a very deep and meaningful conversation with its author…I love the fact that this is not about people living with dementia as somehow different or separate, it is a book about all of us and what it means to be vibrant sexual and sensual beings.’
Reviewed by Anna C. Park. Published by and available from Jessica Kingsley Publishers
Dear Life
by Rachel Clarke
Palliative medicine is Dr Clarke’s second career; her first as a journalist gave her the skills to evoke the kindness, joy and tenderness seen every day in a hospice, where death should dominate yet it is love and life itself that take centre stage.
Described as a love letter – to her GP father dying of cancer, to a profession where Dr Clarke helps people live the end of their lives as fully and richly as possible, to life itself – this is a beautifully written story of love and loss, invoking laughter and tears in equal parts.
Published Jan 30th 2020. Available from Amazon.
Watching the Leaves Dance
by Graham Stokes
As Keith Oliver writes in his Foreword, “Watching the Leaves Dance takes us once again, not into the realm of patients, carers or service users but into the lives of people…”. People, not their dementia, are again at the heart of this next volume of stories by Graham Stokes. People with histories, childhood experiences, family influences, all of which make us the person we become… and who we remain, even if dementia claims us. As Professor Stokes says, ‘dementia care does not exist. Instead, we must accept that we care for people with dementia.”
Professor Stokes has often had to look deep into peoples’ pasts to find the clues to their current behaviour, behaviour that may have been causing significant distress to themselves and those around them. Within each of these eighteen stories there are valuable insights wrapped in humanity: Cathy and Jimmy for example, teach us that good care is not measured by flawless appearances, we learn from Maria to be alert to the potential risks of reminiscence therapy, from Gillian and Spencer that dementia has no bearing on our need for closeness, touch and affection, and from Suzy to check the bus timetable before attempting to impose culture change in a care home. This book has something to say to anyone with even the loosest connections to dementia, and that, after all, is most of us. Be prepared to shed tears.
Published by and available from Hawker Publications Ltd.
Caregiver Carols: A Musical, Emotional Memoir
 by Dr Don Wendorf
by Dr Don Wendorf
Dr Wendorf brings his combined experiences of phsychologist and psychotherapist, musician and caregiver to his wife of 40 years in this moving, informative, creative and practical memoir. Searingly honest at times, the author is prepared to tackle the toughest aspects of being a caregiver: guilt (a ‘good, normal, healthy emotion’), the ongoing sense of bereavement (‘I’ve been in denial about being in mourning’), how to accept help (‘don’t deny other loving people the blessing of being able to serve, comfort, support, help, care for, love and give to you’) and perhaps the toughest one of all, the impact illness can have on a couple’s intimate relationship.
The author blends a mix of song lyric rhyming verses with accompanying prose commentaries to make it easier, more effective and more memorable to get his messages across than the ‘standard didactic approach’. In describing his own emotional struggles as a caregiver, Dr Wendorf hopes to encourage other caregivers that their own feelings are tough but normal and manageable and that they are not alone.
Dementia: The One-Stop Guide
by June Andrews
I’ve had the privilege of hearing Professor June Andrews present at a number of conferences and have always enjoyed her unique mix of down-to-earth practical approach to dementia care and refreshing sense of humour, so I was delighted to see the same attributes appear on the pages of this invaluable book.
Advertised as ‘practical advice for families, professionals, and people living with dementia and Alzheimer’s Disease’, one might think it a little ambitious, attempting to be all things to all people, but I would defy anyone in those groups mentioned to read it and say they learned nothing. No subject is taboo, there’s lots of myth-busting and advice on how to negotiate a system which, the author acknowledges, all too often lets people down, plus comments from carers, professionals and those living with varying forms of dementia. If you’re looking for a jargon-free easy read, packed with practical information for anyone dealing with dementia in the UK and flashes of good humour to lighten the message, this is the book for you.
Click here to purchase from Amazon
On Pluto: Inside the Mind of Alzheimer’s
by Greg O’Brien
Journalist Greg O’Brien writes powerfully about his ten year journey – so far – with Alzheimer’s. There are a number of laugh out loud moments as he paints a vivid picture of his daily struggles to find coping mechanisms and strategies to circumvent the disease that is determined to trip him up, and which will, he knows, eventually send him to Pluto, his allegory for the end stages of Alzheimer’s Disease. On every page O’Brien demonstrates how he is living with dementia, not dying from it.
Click here to purchase from Amazon
The Things Between Us – Living Words: Anthology 1
 “Like dipping into a basin of water, and trying to hold the droplets in your hands as you splash your face with pure joy”. So says the late Lynda Bellingham in her resounding endorsement of this wonderful anthology of poems and words, collected from people living with dementia.
“Like dipping into a basin of water, and trying to hold the droplets in your hands as you splash your face with pure joy”. So says the late Lynda Bellingham in her resounding endorsement of this wonderful anthology of poems and words, collected from people living with dementia.
The charity Living Words has worked with people with dementia since 2007. As Founder and Artistic Director Susanna Howard says, when a person hears their words read back to them their sense of well-being and personhood is elevated…
Click here to purchase from Living Words
Dancing with Dementia
by Christine Bryden
Author Christine Bryden continues to lead an active life and in May 2015 it will be an incredible 20 years since her diagnosis of dementia.
Christine was a top civil servant and single mother of three children when she received her diagnosis at the age of 46. ‘Dancing with Dementia’ is a vivid account of how she dealt with that life-changing news, exploring the effects of memory problems, loss of independence, difficulties in communication and the exhaustion of coping with simple tasks. She describes how, with the support of her husband Paul, she continues to lead an active life despite her dementia and explains how professionals and carers can help.
Click here for further information and ways to purchase.
Person-centred Dementia Care. Making services Better.
by Dawn Brooker
This was the first book I read about dementia care when my husband had to move to a care home in 2009 with advanced dementia and complex needs, and its value and relevance for anyone involved in providing care shone out immediately. Refreshingly honest and down-to-earth, Professor Brooker questions whether all providers who claim to offer person-centred care truly reflect the values that should lie behind this overused and misused term. She describes her book as an attempt to articulate the different elements of person-centred care and to describe what these look like in practice.
Frequently referring to Tom Kitwood as her inspiration, Dawn Brooker explains the four key elements of person centred care that comprise the VIPS model: Valuing people with dementia and those who care for them (V); treating people as Individuals (I); looking at the world from the Perspective of the person with dementia (P); and a positive Social environment in which the person living with dementia can experience relative well being (S).
With an emphasis on practical application, Person Centred Dementia Care provides care organisations with clear, accessible guidelines on how to put the VIPS model into operation for effective care that is `fit for VIPs’. Part 2 of the book comprises the VIPS organisational reflection tool, which care providers can use to assess how well they think they are doing at providing person-centred care.
Click here for further information and to purchase.
The Bright Side / The Other Side
by Kate Granger

Most people reading this will have heard of Dr Kate Granger, and of her struggle to live as normal a life as possible under the shadow of a terminal cancer diagnosis. As famous as the doctor herself is her inspirational ‘#HelloMyNameIs…’ campaign to encourage all health care staff to introduce themselves to their patients before delivering care. As Kate says on her website, introducing oneself is much more than just providing a name: it is making a human connection, beginning a therapeutic relationship, building trust.
Kate’s first book, ‘The Other Side’ is riddled with technical terms and medical-speak, making it quite clear which audience she wants to reach. Self-published, with all profits going to the Yorkshire Cancer Centre and orders being handled by Kate and her husband Chris so as to maximise the revenue for YCC, it reflects very much the author as she describes herself: ‘slightly bossy, competent but compassionate’ and no sign of the person she fears some will see her as: ‘that poor girl dying of cancer’. For us lay people, Kate has thoughtfully provides a glossary of terms, but one doesn’t need to understand the jargon to get the message. This is a doctor telling it how it is on the other side. Or, to put it another way, this is a patient with medical knowledge describing the progression of her illness, details of her treatment, and making it quite clear what worked and what didn’t in the huge variety of approaches and attitudes she experienced from her professional colleagues.
I read both books from cover to cover with barely a break, hauled in trepidation along Kate’s journey with a mixture of emotions, feeling her frustration when the medics got it wrong, delighting with her when she experienced compassionate, kind and intelligent care, reduced to tears when she, rarely, appears overwhelmed by pain and the desperate nature of her situation.
Being able to return to work allowed Kate to put into practice the things she had learned as a patient: proper communication – finding the right balance to avoid being patronising or confusing; getting the little things right such as getting on the same level as your patient when talking to them; remembering that you are treating a human being and not just a medical condition. It is clear from reviews and from Kate’s own comments that doctors and other healthcare staff have also adjusted their behaviour as a result of reading Kate’s books. I’d say they need to be on the compulsory reading list of every single healthcare professional.
This link will take you to Kate’s website where her books are available for purchase.
And Still the Music Plays. Stories of People with Dementia
by Graham Stokes
Dr Graham Stokes has written a number of books on the subject of dementia care, but this is no ordinary instruction manual. Instead, the author recounts 22 compelling stories of people with dementia and looks beyond the obvious in an attempt to explain why some behave in the way they do.
You will read about Mr Abrahams who came alive when touched by human contact, how a window into Mrs S’s world opened when staff came to understand her aversion to shared toilets, and how Lucy’s quality of life was transformed when it was discovered what caused her to shout for hour after hour.
The central theme is that everyone is unique, and it is only by thinking deeply about each person individually that we can give the best possible care.
Click here for further information and to purchase.
Dear Dementia: The laughter and the tears
by Ian Donaghy
As author Ian Donaghy says, “Dementia is an uninvited guest. It does not discriminate and is often merciless… but there is still laughter to be heard.” These short letters and over 100 illustrations, with their simple yet powerful messages, provide many opportunities for people to laugh and to cry, to learn and to ponder. They are based on Ian’s own experiences and conversations with people living with dementia and their friends and family, including children.
This is a delightful book which has at its core a heartfelt plea that we focus on the person and not the dementia.
Click here for further information and to purchase.



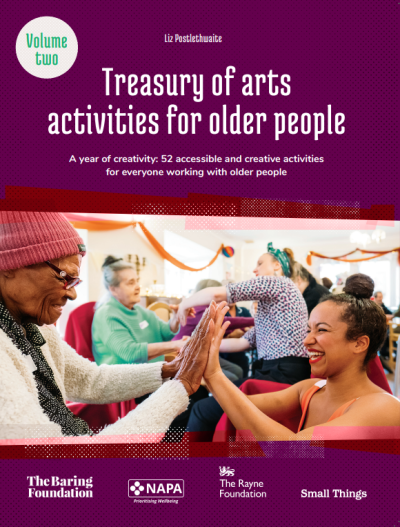
 The National Activity Provider’s Association or NAPA is the UK’s leading activity and engagement charity. Their vision is for the arts and meaningful conversation to become an integral part of care provision so people can live content, creative and connected lives. As a membership organisation they support people to develop the essential knowledge, skills, and confidence required to prioritise wellbeing and provide person-centred activity and engagement. You can find a wealth of useful resources, training opportunities and information about upcoming events on the new NAPA website:
The National Activity Provider’s Association or NAPA is the UK’s leading activity and engagement charity. Their vision is for the arts and meaningful conversation to become an integral part of care provision so people can live content, creative and connected lives. As a membership organisation they support people to develop the essential knowledge, skills, and confidence required to prioritise wellbeing and provide person-centred activity and engagement. You can find a wealth of useful resources, training opportunities and information about upcoming events on the new NAPA website:  Arts in Care Homes is a five year project managed by NAPA and funded by The Baring Foundation and The Rayne Foundation. There is a wealth of arts activities taking place in care homes across England. These range from everyday creative activities run by staff members, including flower arranging, woodwork and watercolour painting to large scale arts projects such as A Choir in Every Care Home.
Arts in Care Homes is a five year project managed by NAPA and funded by The Baring Foundation and The Rayne Foundation. There is a wealth of arts activities taking place in care homes across England. These range from everyday creative activities run by staff members, including flower arranging, woodwork and watercolour painting to large scale arts projects such as A Choir in Every Care Home. This free creative booklet is for care-givers, people living with dementia or long-term health conditions as well as practitioners and professionals working in social/healthcare settings.The booklet is an invitation to take a sensory exploration with those around you, sparking the imagination, keeping minds active and feeling connected. We hope these activities generate inspiration from within your home, and encourage creativity and expression to blossom.
This free creative booklet is for care-givers, people living with dementia or long-term health conditions as well as practitioners and professionals working in social/healthcare settings.The booklet is an invitation to take a sensory exploration with those around you, sparking the imagination, keeping minds active and feeling connected. We hope these activities generate inspiration from within your home, and encourage creativity and expression to blossom. By Liz Postlethwaite, The Baring Foundation
By Liz Postlethwaite, The Baring Foundation This Project began in 2019 as a response to the coronavirus situation. Originally a postal project we now ask pen pal partners to send messages of support, including letters, postcards, artwork and poems to care homes via email. We have already linked up over 300 care homes with Only Connect Pen Pal partners including, artists, art organisations, school children, families and individuals.
This Project began in 2019 as a response to the coronavirus situation. Originally a postal project we now ask pen pal partners to send messages of support, including letters, postcards, artwork and poems to care homes via email. We have already linked up over 300 care homes with Only Connect Pen Pal partners including, artists, art organisations, school children, families and individuals.